Prevalence of Preterm Premature Rupture of Membranes and Its Correlated Risk Factors among Pregnant Women Attending Women Health Hospital, Assiut University, Egypt
Amel Dawod Kamel Gouda1,2*, Reda M Nabil Aboushady1, Amira Elhoufey3,4, Treza Saber Badia5
1Faculty of Nursing, Maternal and New-born Health Nursing, Cairo University, Cairo Governorate 4240310, Egypt
2College of Nursing- King Saud bin Abdul-Aziz University for Health Sciences,22384 Riyadh, Saudi Arabia; King Abdullah International Medical Research Center, Ar Rimayah, 11481 Riyadh, Saudi Arabia
3Faculty of Nursing, Jazan University, Jazan 45142, Saudi Arabia
4Faculty of Nursing, Community Health Nursing, Assiut University, Assiut Governorate 2072350, Egypt
5Faculty of Nursing, Maternal and New-born Health Nursing, Assiut University, Assiut Governorate 2072350, Egypt
*Corresponding Author’s Email: goudaa@ksau-hs.edu.sa
ABSTRACT
Background: Preterm premature rupture of the membrane (PPROM) is an ongoing obstetric issue and presents many interesting research questions. The aim of the current study is to determine the prevalence and correlated risk factors of preterm premature rupture of membranes among pregnant women. And assess the relationships between risk factors and the occurrence of preterm premature rupture of the membrane. Methods: A retrospective cross- sectional research design was adopted. A purposive sample of 100 pregnant women, diagnosed with PPROM and admitted to the labour and delivery room at Women Health Hospital, Assiut University, during the year 2023 was recruited. Two tools were used to collect the current data: 1) Structured Questionnaire and 2) Risk Factors for Preterm Premature Rupture Membrane Assessment Tool. Results: Findings revealed that the mean maternal age was 30.07 ± 5.918. The prevalence of PPROM was 1.85%. There was a statistically significant difference between maternal age, residence, BMI, occupational level, gravidity, parity, gestational age, number of abortions, previous history of PROM, previous mode of delivery, and occurrence of PPROM. Conclusion: The prevalence of PPROM was 1.85%. The risk factors for the occurrence of PPROM were gravidity, parity, gestational age, abortions, and a previous mode of delivery. Recommendation: Enhancing the awareness of maternity nurses and midwives about the importance of assessment and early detection of PPROM as part of routine care for all pregnant women can help reduce its incidence and associated complications.Keywords: Correlated Risk Factors; PPROM; Pregnant Women; Prevalence
INTRODUCTION
The most important role of the foetal membranes is maintaining a safe intrauterine fluid environment until birth begins. Their spontaneous rupture usually happens close to the end of the first stage of labour in around 70% of pregnancies without interventions (Sudha & Biradar,2023). A spontaneous rupture typically happens close to the end of the first stage of labour in approximately 70% of pregnancies that do not include medical interventions. The physiological cause of spontaneous membrane rupture is the membranes’ gradual deterioration with increasing gestational age (Pisoh, 2021).
Preterm premature rupture of membranes (PPROM) is defined as spontaneous leakage of amniotic fluid that happens before 37 weeks of gestation. It accounts for approximately 1% to 5% of pregnancies and accounts for roughly two-thirds of all preterm births; of the 4 million births that occur in the United States each year, PPROM affects over 120,000 pregnancies (Günes et al., 2022). The Indonesia Demographic and Health Survey in 2012 found that the rate of maternal death was 359 per 100,000 live births. Infection was the primary cause of maternal mortality with PPROM (Abebe et al., 2022).
PPROM occurs in 5% to 10% of all deliveries worldwide. The frequency of PPROM varies by country: in China, it is 18.7% (Zhuang et al., 2020); 2.2% in India (Garg & Jaiswal, 2023); 4.91% in Cameroon (Pisoh, 2021); 5.3% in Egypt (Abouseif et al., 2018); 13.8% in Uganda (Byonanuwe et al., 2020); and 23.5% in Ethiopia (Yadeta et al, 2020). Approximately 0.3% to 0.4% of pregnancies result in mid-trimester preterm premature rupture of membranes (PPROM), an infrequent clinical syndrome. In about 38% to 70% of pregnancies with PPROM, delivery normally occurs within the first week of the condition, resulting in the birth of viable foetuses. Pregnancies that continue to have oligohydramnios in the second trimester experience impaired foetal lung development, potentially leading to pulmonary hypoplasia in the future (Celik et al., 2023). Preterm PROM was 2.2%, and the perinatal death rate was 206 per 1,000 babies. The lowest Apgar score in the first minute was the most unfavourable perinatal outcome in this case. The most common neonatal outcome among those referred to the intensive care unit was early-onset neonatal sepsis, followed by respiratory distress syndrome. Additionally, placental abruption was the most common maternal outcome. Early neonatal mortality was the least common neonatal outcome in this study (Abebe et al., 2023).
The rigorous causes of premature rupture of the membrane are unknown. Still, it may occur in conjunction with or apart from group B streptococcal infection, urinary tract infection, and, in other cases, may have early signs of chorioamnionitis. Increase in risk factors with maternal premature rupture of the membrane is as follows: infection, multifetal gestation, maternal smoking, urinary tract infection, and occurrence of cervical incompetence (Enjamo et al., 2022). Prematurity, respiratory distress syndrome, hypoxia, and sepsis are among the neonatal complications linked to early rupture of the membrane (Dayal, Jenkins & Hong, 2023). Scientific documentation revealed that the risk factors for the occurrence of PPROM were as follows: advanced maternal age, low educational attainment, low socioeconomic status, parity, pregnancy-induced hypertension (PIH) (Asefa & Ayele, 2020), urinary tract infection (UTI), history of caesarean section, history of abortion, smoking, and multifetal gestation (Habte, Dessu & Lukas, 2021). Low socioeconomic status, anaemia during pregnancy, lower genital tract infection, urinary tract infection (UTI), prior history of premature rupture of the membrane (PROM), malpresentation, multiple pregnancies, and polyhydramnios have been found to be risk factors linked to PPROM in various studies (Addisu, Melkie & Biru, 2020).
To treat preterm premature rupture of the membranes, it is necessary to weigh the potential benefits for the newborn after extending the gestational period against the risks of intra- amniotic infection and the issues it might cause for the mother and foetus. Gestational age and the existence or absence of chorioamnionitis are two other factors that affect therapy (Singh et al., 2022). According to Bohilțea et al. (2021), pregnant women with PPROM who do not have an infection can be managed with either expectant management or active intervention. Women diagnosed with positive chorioamnionitis will receive active delivery and start antibiotic treatment, regardless of gestational age. Women who are not experiencing labour should also have labour induced to expedite delivery (Sudha & Biradar, 2023).
Maternity nurses play a crucial role in prenatal care. It is essential that the nurse concentrates on enhancing the health of both the pregnant woman and her unborn child. This involves offering not just hands-on nursing assistance but also identifying and managing early risk factors through providing health education and support to pregnant women. Currently, the established norm is to extend foetal gestational age through a full-term pregnancy in order to reduce preterm symptoms, possibly reducing the effects of premature birth. The overseeing of ongoing monitoring for signs of infection is referred to as "expected management" and includes providing psychological support and information to women and their families.
Significance of the Study
PPROM is a global health concern that affects both developed and developing nations. It is one of the most prevalent pregnancy problems (Byonanuwe et al., 2020). It is a major cause of increased mortality and morbidities like lower birth weight and other foetal infections. Apart from its effects on morbidity and mortality rates, it is also noteworthy to mention that PPROM also imposes a heavy financial burden at both individual and societal levels (Freeman et al., 2022). PPROM infections have been known to prolong hospitalisations. As a result, the cost of treatment has been noted to increase across all hospitals. Nevertheless, it is crucial to acknowledge that PPROM, similar to other healthcare-related conditions, can be prevented. The literature review highlighted a limited number of studies conducted in in Egypt and provided insight into the prevalence of PPROM and its associated risk factors. Therefore, the current study aims to determine the prevalence and correlated risk factors of preterm premature rupture of membranes among pregnant women and assess the relationships between these risk factors and the occurrence of PPROM.
Aim of the Study
The research aims to determine the prevalence and correlated risk factors of preterm premature rupture of membrane among pregnant women. It also focuses on assessing relationships between associated risk factors and the occurrence of PPROM.
METHODOLOGY
Research Design
A retrospective cross-sectional research design was employed to assess the risk factors of preterm premature rupture of membranes among pregnant women. This design was chosen for many reasons. First, it allows for the collection of detailed information about the research problem within a limited period. Second, this design helps the researcher study prevalence and the relationships among multiple variables, aligning with the study's aim and objectives. Furthermore, it helped increase understanding of the research problem and the phenomenon under investigation (Ishtiaq, 2019).
Sample
A purposive sample of 100 pregnant women was selected from hospital medical records according to specific inclusion criteria, which included a diagnosis of PPROM and an age range of 18 to 45 years. Pregnant women who experienced membrane rupture after 37 weeks of gestation were excluded from the study.
Sample Size
Between January 2023 and December 2023, approximately 13,469 women sought care at the Women's Health Hospital of Assiut University, with around 5,400 deliveries recorded. During this period, the prevalence of PPROM was estimated at 1.85%.
Setting
The research was carried out at the Women's Health Hospital of Assiut University, Egypt. The building consists of six floors, with five designated for public use and the top floor reserved for private services. Since its establishment in 2005, the Women's Health University Hospital has provided obstetrics and gynaecology services to numerous patients in Upper Egypt. In 2023, approximately 13,469 cases were recorded, including around 5,400 births.
Tools of Data Collection
Two tools were used to collect the current data: a structured questionnaire and a risk factors assessment tool for the occurrence of preterm premature rupture of membranes assessment.
Tool (I): A Structured Questionnaire
This tool was developed by a researcher after an extensive literature review; it consists of two parts. The first part included data related to demographics data, and the second part included data related to previous obstetric data.
Tool (II): Risk Factors for Preterm Premature Rupture of Membrane Assessment Tool This instrument was designed by researchers based on a comprehensive review of the literature (Bouvier et al., 2019; Dayal, Jenkins & Hong, 2023) and consists of three parts. The first part includes data related to medical history, such as the occurrence of previous urinary tract infections, hypertension, preeclampsia, diabetes mellitus, cardiac disease, anaemia, bleeding, obesity, and other medical conditions. The second part includes data related to behavioural history, such as lifting heavy objects, smoking, falling, exercise, type of exercise (walking, swimming, aerobics, other), and nutritional status. The third part includes data related to current obstetric history, such as placental type, multiple pregnancies, malpresentation, malposition, antenatal infection, cervical incompetence, polyhydramnios, oligohydramnios, intrauterine foetal death, intrauterine growth retardation, antenatal care follow-up, and the main reason for PROM in the current pregnancy.
Tool Validity and Reliability
A panel of three experts in the fields of maternity and community health nursing reviewed the tools. The purpose of this evaluation was to assess their relevance, clarity, and content validity, leading to necessary modifications. Cronbach’s alpha test was used to assess the reliability of the tools, with the results indicating that the tools were highly reliable, with a reliability coefficient of 0.78.
Procedure
After obtaining formal clearance from the Director of Women's Health Hospital, the researchers introduced themselves and explained the study's objectives to seek the cooperation of all obstetric nurses. From the total cohort of 5,400 pregnant women who delivered at the Women's Health Hospital of Assiut University during 2023, 100 pregnant women were diagnosed with PPROM. Data were collected from hospital records, and pregnant women who met the inclusion criteria were enrolled in the study. The researchers then examined their hospital patient records using data collection tools, recording all relevant information, including risk factors, medical history, personal details, and prior obstetric history. The instruments were stored in the nursing office of the work unit. Data were collected four days a week over three months, from 1st July to the end of August 2024, with each questionnaire taking 20 to 30 minutes to complete. Confidentiality of the information was ensured.
Statistical Analysis
The data were gathered, tabulated, and statistically analysed using the Statistical Package for Social Sciences (SPSS) version 24. Analytical statistics were employed to examine the relationship between two qualitative variables using the chi-square test. Descriptive statistics, including quantitative data presented as mean (X) and standard deviation (SD), were used, while Pearson’s correlation coefficient (r) was applied to test the correlation between interval and ratio variables. The significance threshold for the analysis was set at 5%, with a p-value of
<0.05 considered statistically significant.
Ethical Considerations
The research obtained ethical clearance from the Research Ethics Committee of the Faculty of Nursing, Assiut University, Egypt with reference number 1120240797 on 28th April, 2024.
RESULTS
According to Figure 1, the prevalence of PPROM in pregnant women who gave birth at Assiut Maternity University Hospital during the study period was 1.85%.
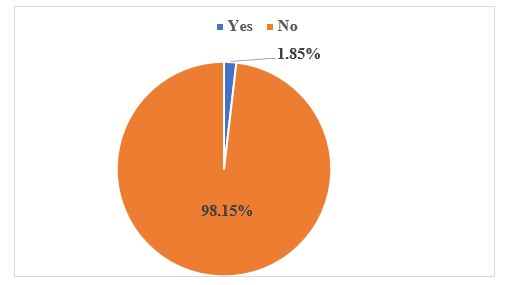
Figure 1: Prevalence of PPROM among Pregnant Women Who Delivered at Assiut Maternity University Hospital over One Year
Table 1: Distribution of the Study Sample Regarding Demographic Characteristics (N=100)
Variable
Frequency
%
Maternal Age
<25 years
19
19
25 to 35 years
68
68
>35 years
13
13
(Mean±SD) Yrs
30.07±5.92
Educational Level
Primary education
4
4
Secondary education
24
24
University education
72
72
Residence
Urban
96
96
Rural
4
4
Occupational Level
Working
8
8
Housewives
92
92
BMI Categories
Normal Weight
8
8
Overweight
20
20
Obesity Class I
47
47
Obesity Class II
18
18
Obesity Class III
7
7
(Mean ± SD) Kg/m²
32.13 ± 5.68
Table 1 displays that the average age of the group was 30.07 years old with a standard deviation of 5.92. Furthermore, 72% of the participants in the study had completed their university education.
Furthermore, 96% of the sample resides in urban areas. Additionally, housewives made up 92% of the participants in the study. The average BMI was 32.13 ± 5.68 kg/m².
Table 2: Distribution of the Study Sample Regarding Lifestyle History (N=100)
Variable
Frequency
%
Lifting Heavy Objects
Yes
6
6
No
94
94
Physical Exercise
No exercise
37
37
Walking exercise
61
61
Swimming
2
2
Nutritional Status
Adequate
97
97
Inadequate
3
3
Table 2 shows that 94% do not lift heavy objects. Among them, 61% reported walking as their preferred form of exercise, while only 3% of the sample exhibited inadequate nutritional status.
Table 3: Distribution of the Study Sample Regarding Current Obstetric History (N=100)
Variable
Frequency
%
Placenta Type
Normal
97
97
Displacement
1
1
Multiple pregnancies
2
2
Mal-presentation
8
8
Malposition
3
3
Antenatal Infection
Group B Streptococcus
2
2
Bacterial vaginosis
2
2
Herpes simplex
1
1
Cervical incompetence
2
2
Polyhydramnios
1
1
Oligohydramnios
12
12
Intrauterine fatal death
1
1
Intrauterine growth retardation
1
1
Antenatal care follow-up
76
76
The Reason for the Rupture of the Membrane
I don't know
42
42
During delivery
22
22
Placenta previa
5
5
Other
9
9
*Number is not exclusive. i.e., each woman gave more than one problem
Table 3 illustrates that 97% of the study sample had normal placentas, 2% had multiple pregnancies, 8% had malpresentation, and 3% of them had malposition. In addition, 2% had antenatal infection group B Streptococcus, and 2% had bacterial vaginosis. Only 1% had cervical incompetence, 1% had polyhydramnios, 12% had oligohydramnios, 0.6% had an intrauterine foetal death, and 1% had intrauterine growth retardation. In addition, 76% had antenatal care follow-up.
Table 4: The Relationship between Risk Factors for PPROM and Their Maternal Age
Risk factors
Chi-Square (2)
P-value
Medical history
15.68
0.001**
Lifting heavy objects
2.531
0.470
Physical exercise
14.45
0.04*
Nutritional status
0.864
0.834
Placenta type
2.631
0.452
Multiple pregnancies
2.253
0.522
Mal-presentation
0.670
0.880
Malposition
0.735
0.865
Antenatal infection
0.168
0.983
Cervical incompetence
12. 06
0.005**
Polyhydramnios
0.866
0.834
Oligohydramnios
1.469
0.689
Intrauterine fatal death
3.729
0.292
Intrauterine growth retardation
3.122
0.373
Antenatal care follow-up
0.569
0.903
*Statistically significant differences- ** Highly statistically significant differences
Table 4 shows statistically significant relationship between risk factors for occurrence of PPROM and medical history (2=15.88, i=0.001), physical exercise (2=14.45, p=0.04), cervical incompetence (2=12.06, p=0.005). While there was no relationship between occurrences of PPROM and lifting heavy objects, nutritional status, placental type, multiple pregnancies, mal-position, mal-presentation, antenatal infection, polyhydramnios, oligohydramnios, Intrauterine Foetal Demise (IUFD), Intrauterine Growth Restriction (IUGR), and antenatal care follow-up.
Table 5: The Relationship between Maternal Demographic Characteristics and Occurrence of PPROM
Variables
Risk factors for Premature Rupture of Membrane
Test
P
Maternal age
r= 0.337
0.0001**
BMI
r= 0.197
0.013*
Educational level
F= 2.046
0.133
Residence
T=6.903
0.009*
Occupational level
F=3.202
0.043*
**Highly Statistically Significant Differences, * Statistically Significant Differences
Table 5 shows a statistically significant relationship between risk factors for the occurrence of PPROM and maternal age (r = 0.337, p = 0.0001); BMI categories (r = 0.197, p = 0.013); residence (T = 6.903, p = 0.009); and occupational level (F = 3.202, p = 0.043). While there was no relationship between risk factors of occurrences of PPROM and educational level.
Table 6: The Relationship between Obstetrical Profile and Occurrence of PPROM
Variables
Risk factors
Test
P
Gravidity
r= 0.333
0.0001**
Parity
r= 0.311
0.0001**
Gestational age in a week
r= 0.195
0.013*
Number of abortions
r= 0.229
0.004**
Previous history of PPROM
T=0.377
0.562
Previous preterm labour
T= 0.009
0.926
The previous mode of delivery
F=2.845
0.040*
**Highly Statistically Significant Differences- * Statistically Significant Differences
Table 6 presents a significant correlation between PPROM and gravidity (r=0.333, p=0.001); parity (r=0.311, p=0.001); gestational age in a week (r=0.195, p=0.013); number of abortions (r=0.229, p=0.004); and previous mode of delivery (r=0.369, p=0.001). Although there was no clear relation between past PPROM history and preterm labour, as well as risk factors for developing PPROM.
DISCUSSION
This section analyses with the study findings in three parts: 1) the prevalence of PPROM among the study sample, 2) the risk factors for the occurrence of PPROM in the study sample, and 3) the correlation between maternal demographics, obstetric profile, and the occurrence of PPROM.
Prevalence of PPROM among the Study Sample
The current research was conducted at Maternity University Hospital in Assiut Governorate, which provides specialised medical care for the entire region, with around 5,400 deliveries between July 2022 and August 2023. A total of one hundred expectant mothers with PPROM (1.85%) were part of the study. In contrast, another research conducted in Egypt aimed to assess the occurrence and outcomes for both the foetus and mother of early rupture of membranes in pregnant women receiving care at Minia Maternity University Hospital. They stated that the rate of PPROM among women who gave birth at Minia Maternity University Hospital during the study timeframe was 7.4% (Ali, Abd-El-Kader & Mansour, 2020). The increased rate at Minia Maternity University Hospital may be attributed to birth spacing practices, low maternal weight growth caused by poverty, and cultural effects on early marriage, all of which are strongly linked to PPROM. This theory was supported by Rattan and Ramnarain (2024). On the other hand, research conducted by González-Mesa et al. (2021) found that Malaga University Regional Hospital assisted a total of 119,888 deliveries from 2000 to 2020. Out of those, 14,931 were born before 37 weeks, and there were 4,591 instances of PPROM identified. These accounted for 3.8% of all births attended and 30.7% of all preterm deliveries. A total of 592 deliveries (making up 0.5% of all deliveries, 3.9% of all preterm births, and 12.9% of all cases of PPROM) took place in pregnancies at or before 28 weeks. This could be clarified by the prevalence seen in a study carried out in a developed country with a stronger emphasis on delivering quality care compared to a developing country.
Risk Factors for the Occurrence of PPROM among the Study Sample
PPROM is a medical issue that leads to the early deterioration and breaking of the foetal membranes before the start of labour. The cause of PPROM seems to have multiple factors, including demographics and clinical aspects like smoking, low socioeconomic status, prior preterm birth, excessive stretching of membranes, connective tissue disorders, past cervical surgery, and choriodecidual infection. Numerous risk factors are associated with PPROM. In the current findings, it was reported that there was a statistically significant relationship between risk factors for the occurrence of PPROM, maternal age, medical history (2= 15.88, p = 0.001), physical exercise (2= 14.45, p = 0.04), and cervical incompetence (2= 12.06, p = 0.005). However, there was no relationship between risk factors for the occurrence of PPROM and lifting a heavy object, nutritional status, placental type, multiple pregnancies, malposition, malpresentation, antenatal infection, polyhydramnios, oligohydramnios, intrauterine foetal demise (IUFD), intrauterine growth restriction (IUGR), and antenatal care follow-up. The findings of the current study are in line with Habte, Dessu and Lukas (2021) and Lin et al. (2024), where most of their study sample had no history of heavy object lifting.
In a comparable study conducted by Bouvier et al. (2019), a prospective cohort of 6,968 pregnant women was analysed to assess the risk factors and outcomes associated with preterm premature rupture of membranes (PPROM). According to their research, maternal age, smoking, poor annual income, higher BMIs, and a 60-month gap between pregnancies are all linked to an elevated risk of PPROM.
Additionally, a statistically significant correlation between PPROM and body mass index and educational status was found in the current study. The findings indicate that pregnant women with an elevated BMI have a statistically significant likelihood of experiencing pre-existing medical conditions, fetal malpresentation, and intrauterine growth restriction, which may increase their risk of developing PPROM. Several studies in the literature have also linked BMI to the occurrence of PPROM. In their study, Mitchell et al. (2021) indicated that there is a statistically significant correlation between BMI and the occurrence of PPROM. The results of this study also show that pregnant women who have fewer educational attainments are more likely to become pregnant more than once, which increases their risk of developing PPROM. Darine, Nabil and Hamouda (2021) confirmed these findings, highlighting an association between low maternal literacy rates and unfavourable maternal outcomes, including preterm premature rupture of membranes (PPROM).
Moreover, bacterial infection is the primary factor linked to the occurrence of PPROM, triggering the decidua and amniotic membranes to release pro-inflammatory cytokines, along with various bioactive substances such as prostaglandins and metalloproteases. Prostaglandins stimulate uterine contraction, while metalloproteases relax and soften the cervix, resulting in membrane rupture. The results in line with Saghafi et al. (2018) that linked antenatal infections like Trichomonas vaginitis, bacterial vaginitis, and Group B Streptococcus to PPROM in expectant mothers. Additional research has also shown that foetal malpresentation, as well as cervical incompetence (Bouvier et al., 2019), are linked to the onset of PPROM.
The findings of the current study showed a relationship between selected maternal demographic characteristics and the occurrence of PPROM. There was a statistically significant relationship between risk factors for the occurrence of PPROM and maternal age (r = 0.337, p = 0.0001); BMI variable (r = 0.197, p = 0.013); residence (T = 6.903, p = 0.009); and occupational level (F = 3.202, p = 0.043). Nonetheless, no correlation was found between the educational level and risk variables for PPROM occurrences. According to this study, obesity is one of the variables linked to a higher risk of PPROM (x = 15.68, p = 0.001). The obesity data in this study were derived from BMI calculations. Maternal obesity has been associated with increased systemic inflammation and an elevated risk of preterm premature rupture of membranes (PPROM) (Mitchell et al., 2021).
Several studies have shown that maternal age is directly correlated with reproductive functions in females (Mehari et al., 2020). For instance, advanced maternal age negatively affects fertility by reducing the quantity and quality of ovum production, leading to congenital abnormalities, distorted intrauterine foetal growth, and PPROM. The findings of this study regarding the association between maternal age and premature rupture of membranes (PROM) align with those of Mahjabeen, Nasreen and Shahreen (2021), who also identified a statistically significant correlation between maternal age and PROM.
A Correlation between Maternal Demographic, Obstetrical Profile, and Occurrence of PPROM
Findings of the current study revealed that there was a statistically significant relationship between the occurrence of PPROM and gravidity (r = 0.333, p = 0.001); parity (r = 0.311, p = 0.001); gestational age in weeks (r = 0.195, p = 0.013); number of abortions (r = 0.229, p = 0.004); and previous mode of delivery (r = 0.369, p = 0.001). However, there was no significant relationship between previous history of PPROM and previous preterm labour and the risk factors for the occurrence of PPROM.
In addition, current study reveals that the more a woman's gravidity had past medical histories and cervical incompetence, predisposition for PPROM. This may be related to gravidity, especially those that lead to birth, can widen the cervix, leading to cervical incompetence (Wang et al., 2024). In the same line, parity means that the study sample had multiple pregnancies and is also likely to have past medical problems and occurrence of PPROM. Findings from this study established a statistically significant relationship between parity and PPROM. Finally, the study shows that a woman with a previous history of PPROM is likely to have medical issues and mal-presentation, and if she has previous preterm labor, she is likely to have past medical issues. Similarly, the previous moods of delivery also significantly influence placenta type.
Limitation
In the present study data collection was difficult due to the hospital's reliance on paper-based medical records. Additionally, inconsistent availability of administrative personnel further restricted access to these records. The absence of an electronic medical record system added complexity to case identification and data retrieval. Future studies would benefit from utilizing digital health records to enhance data accessibility, accuracy, and efficiency in research.
CONCLUSION
The results of the study revealed that preterm premature rupture of membranes (PPROM) was observed in 1.85% of the participants. The research identified several factors that contribute to an increased risk of PPROM, including maternal age, a sedentary lifestyle, cervical incompetence, body mass index (BMI), place of residence, and occupational status. Moreover, significant relationships were observed between the number of pregnancies, number of births, length of pregnancy, abortions, and previous mode of delivery and the occurrence of PPROM. These findings highlight the importance of early screening and targeted interventions to reduce the risk and complications associated with PPROM, ultimately improving maternal and neonatal outcomes. Enhancing maternal care strategies can ultimately improve both maternal and neonatal outcomes.
Recommendation
Pregnant women should be enlightened about the various risk factors of PPROM through health education programs that must be introduced in antenatal outpatient clinics by maternity nurses. Healthcare professionals, as well as midwives and maternity nurses, should consider maternal socioeconomic and obstetric factors as potential indicators for PPROM when evaluating pregnant women at their prenatal appointments. All hospital records should be electronic.
A large-scale cohort study involving prenatal women should be conducted to identify asymptomatic individuals at risk of PPROM. This research could contribute to the development of a clinically relevant predictive model. Additionally, a more comprehensive analytical investigation with a larger sample size should be undertaken to identify other potential risk factors for PPROM.
Conflict of Interest
The authors declare that they have no competing interests.
ACKNOWLEDGEMENT
The authors are thankful to the institutional authority for completion of the work.
REFERENCES
Abebe, T. A., Nima, D. D., Mariye, Y. F., & Leminie, A. A. (2022). Determinants for perinatal adverse outcomes among pregnant women with preterm premature rupture of membrane: A prospective cohort study. Frontiers in Reproductive Health, 4. https://doi.org/10.3389/frph.2022.1052827
Abebe, T., Nima, D., Mariye, Y., & Leminie, A. (2024). The magnitude of maternal and neonatal adverse outcomes associated with preterm premature rupture of membrane: A prospective cohort study. Journal of Neonatal Nursing, 30(4), 342-348. https://doi.org/10.1016/j.jnn.2023.11.003
Abouseif, H. A., Mansour, A. F., Hassan, S. F., & Sabbour, S. M. (2018). Prevalence and outcome of preterm premature rupture of membranes (PPROM) among pregnant women attending Ain Shams maternity hospital. Egyptian Journal of Community Medicine, 36(2), 99- 107. https://10.21608/ejcm.2018.11055
Addisu, D., Melkie, A., & Biru, S. (2020). prevalence of preterm premature rupture of membrane and its associated factors among pregnant women admitted in Debre Tabor General hospital, northwest Ethiopia: institutional-based cross-sectional study. Obstetrics and Gynecology International, 2020(1). https://doi.org/10.1155/2020/4034680
Ali, M. M., Abd-El-Kader, A. A., & Mansour, M. (2020). Prevalence, fetal and maternal outcomes of premature rupture of membranes among pregnant women attending Minia Maternity University hospital: a prospective study. Minia Journal of Medical Research, 31(3), 329-333. https://doi.org/10.21608/MJMR.2022.220312
Asefa, U., & Ayele, W. M. (2020). Adverse obstetrical and perinatal outcomes among advanced age pregnant mothers in northeast Ethiopia: a comparative cross-sectional study. International Journal of Women's Health, 12, 1161–1169.https://doi.org/10.2147/IJWH.S284124.
Bohilțea, R. E., Cioca, A. M., Dima, V., Ducu, I., Grigoriu, C., Varlas, V., & Furtunescu, F. (2021). Expectant management of PPROM improves neonatal outcome-a retrospective study of 562 patients. Journal of Clinical Medicine, 11(1). https://doi.org/10.3390/jcm11010214
Bouvier, D., Forest, J. C., Blanchon, L., Bujold, E., Pereira, B., Bernard, N., ... & Giguère, Y. (2019). Risk factors and outcomes of preterm premature rupture of membranes in a cohort of 6968 pregnant women prospectively recruited. Journal of Clinical Medicine, 8(11), https://doi.org/10.3390/jcm8111987
Byonanuwe, S., Nzabandora, E., Nyongozi, B., Pius, T., Ayebare, D. S., Atuheire, C., ... & Ssebuufu, R. (2020). Predictors of premature rupture of membranes among pregnant women in rural Uganda: a cross‐sectional study at a Tertiary teaching hospital. International Journal of Reproductive Medicine, 2020(1). https://doi.org/10.1155/2020/1862786
Celik, E., Yildiz, A. B., Guler Cekic, S., Unal, C., Ayhan, I., Melekoglu, R., & Gursoy, T. (2023). Amnioinfusion vs. standard management for the second trimester PPROM: a systematic review and meta-analysis of observational studies and RCTs. The Journal of Maternal-Fetal & Neonatal Medicine, 36(2). https://doi.org/10.1080/14767058.2023.2230511
Darine, S. D., Nabil, S. N., & Hamouda, B. H. (2021). Association between genital tract infection and premature rupture of membranes: A retrospective case-control study in Tunisia, North Africa. African Journal of Reproductive Health, 25(2), 131–137.https://doi.org/10.29063/ajrh2021/v25i2.13
Dayal, S., Jenkins, S. M., & Hong, P. L. (2024). Preterm and term prelabor rupture of membranes (PPROM and PROM). StatPearls Publishing, United States.
Enjamo, M., Deribew, A., Semagn, S., & Mareg, M. (2022). Determinants of premature rupture of membrane (PROM) among pregnant women in Southern Ethiopia: a case-control study. International Journal of Women’s Health, 14, 455–466.https://doi.org/10.2147/IJWH.S352348
Freeman, S.W., Denoble, A.E., Kuller, J.A., Ellestad, S., & Dotters-Katz, S.K. (2022). Management of preterm premature rupture of membranes in the late preterm period.Obstetrical & Gynecological Survey, 77, 283 - 292.https://doi.org/10.1097/OGX.0000000000001024
Garg, A., & Jaiswal, A. (2023). Evaluation and management of premature rupture of membranes: a review article. Cureus, 15(3). https://doi.org/10.7759/cureus.36615.
González-Mesa, E., Blasco-Alonso, M., Benítez, M. J., Gómez-Muñoz, C., Sabonet-Morente, L., Gómez-Castellanos, M., Ulloa, O., González-Cazorla, E., Puertas-Prieto, A., Mozas- Moreno, J., Jiménez-López, J., & Lubián-López, D. (2021). Obstetric and perinatal outcomes after very early preterm premature rupture of membranes (PPROM)-a retrospective analysis over the period 2000–2020. Medicina, 57(5), 469. https://doi.org/10.3390/medicina57050469
Günes, A., Kiyak, H., Yüksel, S., Bolluk, G., Erbiyik, R. M., & Gedikbasi, A. (2022). Predicting previable preterm premature rupture of membranes (pPPROM) before 24 weeks: maternal and fetal/neonatal risk factors for survival. Journal of Obstetrics and Gynaecology, 42(4), 597-606. https://doi.org/10.1080/01443615.2021.1935818
Habte, A., Dessu, S., & Lukas, K. (2021). Determinants of premature rupture of membranes among pregnant women admitted to public hospitals in Southern Ethiopia, 2020: A hospital- based case–control study. International Journal of Women's Health, 613-626.https://doi.org/10.2147/IJWH.S314780
Ishtiaq, M. (2019). Book Review Creswell, JW (2014). Research design: qualitative, quantitative and mixed methods approaches. Thousand Oaks, CA: Sage. English Language Teaching, 12(5), 40. https://doi.org/10.5539/elt.v12n5p40
Lin, D., Hu, B., Xiu, Y., Ji, R., Zeng, H., Chen, H., & Wu, Y. (2024). Risk factors for premature rupture of membranes in pregnant women: a systematic review and meta-analysis. BMJ Open, 14(3). https://doi.org/10.1136/bmjopen-2023-077727
Mahjabeen, N., Nasreen, S. Z. A., & Shahreen, S. (2021). The prevalence of premature rupture of membranes (PROM) in anemic and non-anemic pregnant women at a tertiary level hospital. European Journal of Medical and Health Sciences, 3(4), 25–27.https://doi.org/10.24018/ejmed.2021.3.4.934
Mehari, M. A., Maeruf, H., Robles, C. C., Woldemariam, S., Adhena, T., Mulugeta, M., ... & Kumsa, H. (2020). Advanced maternal age pregnancy and its adverse obstetrical and perinatal outcomes in Ayder comprehensive specialized hospital, Northern Ethiopia, 2017: a comparative cross-sectional study. BMC Pregnancy and Childbirth, 20, 1-10.https://doi.org/10.1186/s12884-020-2740-6
Mitchell, C. J., Darling, A. J., Zemtsov, G., Dillon, J., & Dotters-Katz, S. (2021). 152 Impact of maternal obesity on PPROM latency. American Journal of Obstetrics & Gynecology, 224(2), S104-S105. https://doi.org/10.1016/j.ajog.2020.12.174
Pisoh, D. W., Mbia, C. H., Takang, W. A., Djonsala, O. G. B., Munje, M. C., Mforteh, A. A., ... & Leke, R. J. I. (2021). Prevalence, risk factors and outcome of Preterm premature rupture of membranes at the Bamenda Regional Hospital. Open Journal of Obstetrics and Gynecology, 11(3), 233-251. https://doi.org/10.4236/ojog.2021.113023
Rattan, R., & Ramnarain, H. (2024). Determinants of preterm premature rupture of membranes and associated perinatal and maternal outcomes at General Justice Gizenga Mpanza Hospital, South Africa. African Journal of Reproductive Health, 28(2). https://doi.org/10.29063/ajrh2024/v28i2.3
Saghafi, F., Mirzaie, F., Gorji, E., Nabimeybodi, R., Fattahi, M., Mahmoodian, H., & Zareshahi, R. (2021). Antibacterial and anti-Trichomonas Vaginalis effects of Rosa Damascena mill petal oil (a persian medicine product), aqueous and hydroalcoholic extracts. BMC Complementary Medicine and Therapies, 21, 1-10. https://doi.org/10.1186/s12906-021- 03434-8
Singh, N., Pattnaik, L., Panda, S. R., Jena, P., & Panda, J. (2022). Fetomaternal outcomes in women affected with preterm premature rupture of membranes: an observational study from a tertiary care center in eastern India. Cureus, 14(5). https://doi.org/10.7759/cureus.25533
Sudha, R., & Biradar, P. (2023). Maternal and perinatal outcome in preterm premature rupture of membranes. Int J Reprod Contracept Obstet Gynecol, 12(3), 706-10. https://doi.org/10.18203/2320-1770.ijrcog20230542
Wang, Z., Xiu, X., Zhong, L., Wang, Y., Fang, Z., Lin, S., & Huang, H. (2024). Significance of cervical secretion culture in predicting maternal and fetal outcome in pregnant women with premature rupture of membranes: a retrospective cohort study. Frontiers in Pharmacology, 15. https://doi.org/10.3389/fphar.2024.1328107
Yadeta, T. A., Egata, G., Seyoum, B., & Marami, D. (2020). Khat chewing in pregnant women associated with prelabor rupture of membranes, evidence from eastern Ethiopia. Pan African Medical Journal, 36(1). https://doi.org/10.11604/pamj.2020.36.1.22528
Zhuang, L., Li, Z. K., Zhu, Y. F., Ju, R., Hua, S. D., Yu, C. Z., Li, X., Zhang, Y. P., Li, L., Yu, Y., Zeng, W., Cui, J., Chen, X. Y., Baoan, S., & Feng, Z. C. (2020). The correlation between prelabour rupture of the membranes and neonatal infectious diseases, and the evaluation of guideline implementation in China: A multi-centre prospective cohort study. The Lancet Regional Health – Western Pacific, 3. https://doi.org/10.1016/j.lanwpc.2020.100029
Variable
Frequency
%
Maternal Age
<25 years
19
19
25 to 35 years
68
68
>35 years
13
13
(Mean±SD) Yrs
30.07±5.92
Educational Level
Primary education
4
4
Secondary education
24
24
University education
72
72
Residence
Urban
96
96
Rural
4
4
Occupational Level
Working
8
8
Housewives
92
92
BMI Categories
Normal Weight
8
8
Overweight
20
20
Obesity Class I
47
47
Obesity Class II
18
18
Obesity Class III
7
7
(Mean ± SD) Kg/m²
32.13 ± 5.68
Variable
Frequency
%
Lifting Heavy Objects
Yes
6
6
No
94
94
Physical Exercise
No exercise
37
37
Walking exercise
61
61
Swimming
2
2
Nutritional Status
Adequate
97
97
Inadequate
3
3
Variable
Frequency
%
Placenta Type
Normal
97
97
Displacement
1
1
Multiple pregnancies
2
2
Mal-presentation
8
8
Malposition
3
3
Antenatal Infection
Group B Streptococcus
2
2
Bacterial vaginosis
2
2
Herpes simplex
1
1
Cervical incompetence
2
2
Polyhydramnios
1
1
Oligohydramnios
12
12
Intrauterine fatal death
1
1
Intrauterine growth retardation
1
1
Antenatal care follow-up
76
76
The Reason for the Rupture of the Membrane
I don't know
42
42
During delivery
22
22
Placenta previa
5
5
Other
9
9
Risk factors
Chi-Square (2)
P-value
Medical history
15.68
0.001**
Lifting heavy objects
2.531
0.470
Physical exercise
14.45
0.04*
Nutritional status
0.864
0.834
Placenta type
2.631
0.452
Multiple pregnancies
2.253
0.522
Mal-presentation
0.670
0.880
Malposition
0.735
0.865
Antenatal infection
0.168
0.983
Cervical incompetence
12. 06
0.005**
Polyhydramnios
0.866
0.834
Oligohydramnios
1.469
0.689
Intrauterine fatal death
3.729
0.292
Intrauterine growth retardation
3.122
0.373
Antenatal care follow-up
0.569
0.903
Variables
Risk factors for Premature Rupture of Membrane
Test
P
Maternal age
r= 0.337
0.0001**
BMI
r= 0.197
0.013*
Educational level
F= 2.046
0.133
Residence
T=6.903
0.009*
Occupational level
F=3.202
0.043*
Variables
Risk factors
Test
P
Gravidity
r= 0.333
0.0001**
Parity
r= 0.311
0.0001**
Gestational age in a week
r= 0.195
0.013*
Number of abortions
r= 0.229
0.004**
Previous history of PPROM
T=0.377
0.562
Previous preterm labour
T= 0.009
0.926
The previous mode of delivery
F=2.845
0.040*